Injections
Regenexx SCP (Super Concentrated Plasma) is a concentrated, purified form of Platelet Rich Plasma (PRP) that is made by hand.
This process is undertaken by a technician who has been trained by the senior call biologist at Regenexx headquarters in Denver. Regenexx SCP contains many more platelets than other commercially available forms of PRP made using kits or automated machines and is free of red or white blood cell contamination.
The patient procedure is the same as for PRP, but more blood is required. When it is being processed a technician performs every step manually ensuring the PRP mixture is as pure and free of contaminants as possible.
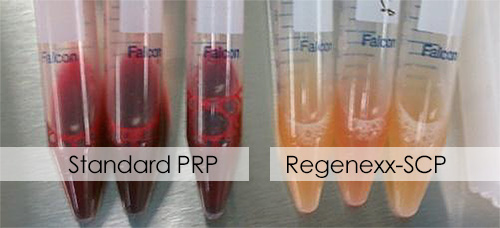
Regenexx-PRP is free of red or white blood cell contamination
How can PRP help me?
PRP has been shown to help relieve pain by assisting the healing process of musculoskeletal tissues. It can help reduce pain due to osteoarthritis, and assists with healing of injuries to the knee, shoulder and hip.
PRP has been shown to delay the progression of early-stage osteoarthritis and relieve the symptoms for up to 12 months. Higher concentrations of PRP appear to have more beneficial effects.
PRP has been shown to assist with healing in both ligament injuries such as ankle sprains[1,2], and tendon injuries such as patella tendinitis[3] and tennis elbow[4].
Most commercial machines that produce PRP can concentrate platelets to about 4 to 5 times the level found in whole blood whilst the Regenexx SCP process can easily concentrate to 16 to 20 times the level found in whole blood, if needed. Also, because each dose is made by hand in a laboratory there is no contamination with red or white blood cells, both of which can stimulate damaging inflammation when released into a joint.
Each dose is individually tailored to each patient, taking into account their age and the target tissue treated.
How much time does PRP treatment take?
Regenexx SCP takes about an hour to produce once the blood has been drawn. It can be injected back into the area of need as soon as it is ready, or stored for injection later in the day.
It is advisable not to do too much activity for the rest of the day but patients can drive to and from the appointment and attend to their own care.
Patients can resume their normal sporting activities within the next few days with maximal pain relief appearing after 10 days in joints and a few weeks in soft tissue injuries.
You don't have to live with an injury or pain. Contact us to find out if a PRP / SCP procedure is suitable for your condition.
Treatment of lateral ankle sprain with platelet-rich plasma: A randomized clinical study. Blanco-Rivera J, Elizondo-Rodríguez J, Simental-Mendía M, Vilchez-Cavazos F, Peña-Martínez VM, Acosta-Olivo C. Foot Ankle Surg. 2020 Oct;26(7):750-754. doi: 10.1016/j.fas.2019.09.004. Epub 2019 Sep 28. PMID: 31640921.
Plasma rich in growth factors (PRGF) as a treatment for high ankle sprain in elite athletes: a randomized control trial. Laver L, Carmont MR, McConkey MO, Palmanovich E, Yaacobi E, Mann G, Nyska M, Kots E, Mei-Dan O. Knee Surg Sports Traumatol Arthrosc. 2015 Nov;23(11):3383-92. doi: 10.1007/s00167-014-3119-x. Epub 2014 Jun 18. PMID: 24938396.
Platelet-rich plasma as a treatment for chronic patellar tendinopathy: comparison of a single versus two consecutive injections. Zayni R, Thaunat M, Fayard JM, Hager JP, Carrillon Y, Clechet J, Gadea F, Archbold P, Sonnery Cottet B.Muscles Ligaments Tendons J. 2015 Jul 3;5(2):92-8. PMID: 26261787; PMCID: PMC4496024.
Platelet-rich plasma (PRP) as therapy for cartilage, tendon and muscle damage - German working group position statement. Tischer T, Bode G, Buhs M, Marquass B, Nehrer S, Vogt S, Zinser W, Angele P, Spahn G, Welsch GH, Niemeyer P, Madry H. J Exp Orthop. 2020 Sep 3;7(1):64. doi: 10.1186/s40634-020-00282-2. PMID: 32885339; PMCID: PMC7471237.
For all appointments and enquiries
OnePointHealth
510/536 High St
Penrith NSW 2750
© 2019-2024 Regenexx Australia